Transforming UK Healthcare Through the Implementation of Digital Twins
Digital twins are fundamentally changing the landscape of healthcare in the UK, presenting extraordinary opportunities for enhancing patient outcomes and increasing operational efficiency. This groundbreaking technology enables the development of virtual replicas of both patients and healthcare systems, which can be meticulously analysed and manipulated to support improved decision-making processes and optimised workflows. With the NHS leading the charge in this digital revolution, the advantages of innovating with healthcare digital twins are becoming ever more evident, marking a significant transformation in the delivery of healthcare services across the nation.
Revolutionising Patient Care with Digital Twin Technology
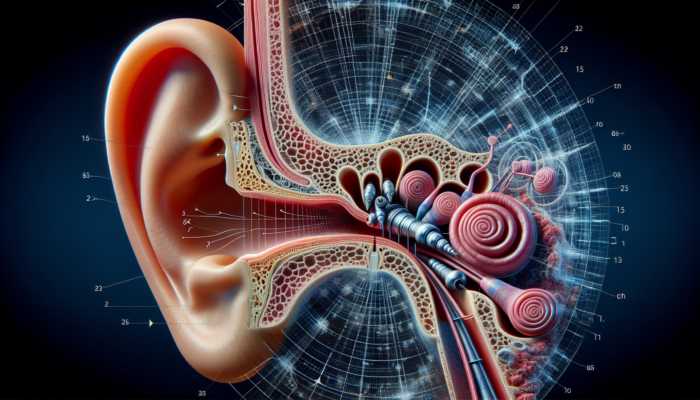
The incorporation of digital twins into patient care has the potential to be profoundly transformative. By constructing personalised models that accurately represent a patient’s unique physiological characteristics and medical history, healthcare professionals can meticulously customise treatment plans tailored to individual requirements. This level of personalisation is achieved through comprehensive real-time data analysis, which takes into account a myriad of factors, including genetics, lifestyle choices, and pre-existing health conditions. As a result, healthcare providers can employ a more precise methodology in treatment, thereby significantly improving patient outcomes.
Recent investigations have underscored the efficacy of personalised treatment plans developed through digital twin technology. For example, a study undertaken at a prominent London hospital revealed that patients suffering from chronic heart conditions exhibited remarkable improvements when their care was managed through digital twin models. These virtual simulations enabled clinicians to predict patient responses to various interventions, ultimately leading to more successful health outcomes. This data-driven method not only enhances care quality but also strengthens the bond between patients and clinicians, as patients feel more actively involved in their treatment journeys.
Furthermore, digital twins are instrumental in facilitating proactive healthcare interventions. By consistently monitoring a patient’s health through their digital twin, healthcare providers can detect potential issues before they escalate into serious problems. This proactive approach allows for timely interventions, which can significantly reduce hospital admissions and, in turn, alleviate the burden on the NHS. Such advancements are particularly vital in light of the increasing demand for healthcare services, ensuring the system can continue to deliver high-quality care to every patient.
Optimising Healthcare Operations with Digital Twin Innovations
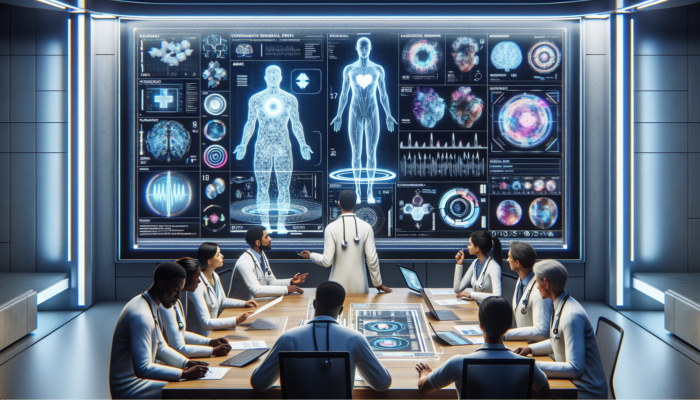
Optimising hospital workflows presents another critical advantage of innovating with healthcare digital twins. By simulating patient flows and interactions within healthcare facilities, digital twins can pinpoint bottlenecks and inefficiencies in real-time. This valuable insight empowers hospital administrators to enact changes that enhance resource allocation and minimise patient wait times.
Consider the implementation of digital twin technology at a notable NHS hospital in Manchester. The facility developed a digital twin of its emergency department, enabling staff to visualise patient journeys and identify key areas for enhancement. By assessing the flow of patients from their arrival to treatment, the hospital successfully reduced waiting times and significantly improved the overall patient experience. This level of insight not only benefits patients but also alleviates pressure on healthcare professionals, allowing them to concentrate on delivering high-quality care.
Moreover, the capacity to model various scenarios using digital twins provides hospital managers with a vital tool for informed decision-making. For example, if a hospital anticipates an influx of patients during flu season, it can utilise its digital twin to simulate different staffing and resource allocation strategies to identify the most effective methods. This foresight and preparation for potential challenges is invaluable in an ever-evolving healthcare landscape.
Ensuring Reliable Medical Equipment Through Predictive Maintenance
Digital twins also play a crucial role in the predictive maintenance of medical equipment, ensuring reliability and minimising downtime. By modelling the operational performance of devices such as MRI machines or ventilators, healthcare providers can monitor their functionality in real-time. This proactive maintenance approach allows for early identification of potential failures, enabling timely scheduling of repairs at convenient times.
For instance, a recent initiative at a hospital in London successfully employed digital twins to monitor the performance of its imaging equipment. By analysing usage patterns and wear-and-tear data, the hospital could anticipate when machines would require maintenance, thus leading to fewer unexpected breakdowns. This proactive strategy not only reduces costs associated with emergency repairs but also guarantees that essential medical equipment is accessible when required, ultimately enhancing patient care.
Furthermore, with an increasing reliance on technology within healthcare, the significance of maintaining medical equipment cannot be overstated. Digital twins facilitate a data-driven approach to equipment management, allowing hospitals to extend the lifespan of their assets and improve their return on investment. As the NHS continues to embrace these technological advancements, integrating digital twins into equipment maintenance strategies will likely become a standard practice nationwide.
Government Initiatives and Policies Supporting Digital Twin Adoption in the UK

The UK government has acknowledged the transformative potential of digital twins in healthcare and is investing in initiatives to support this technological evolution. From strategic plans within the NHS to funding opportunities for innovative projects, the government is playing a central role in facilitating the widespread adoption of digital twin technology within the healthcare sector.
Comprehensive NHS Digital Transformation Strategy
The NHS Digital Transformation Strategy constitutes a thorough plan aimed at harnessing the power of digital technologies, including innovating with healthcare digital twins, to enhance healthcare delivery throughout the UK. This strategy encompasses a range of initiatives designed to improve patient care, streamline operations, and bolster the overall efficiency of NHS services.
At the core of this strategy lies a commitment to integrating data-driven decision-making into everyday healthcare practices. Digital twins are viewed as essential to achieving this objective, as they furnish healthcare professionals with the insights necessary to make informed decisions regarding patient treatment and resource management. By embracing digital twin technology, the NHS aspires to elevate patient experiences, decrease administrative burdens, and cultivate a more agile healthcare system.
Evidence of the implementation of this strategy can be observed in various projects across the UK. For example, several NHS trusts are piloting digital twin programmes aimed at optimising surgical planning and enhancing post-operative care. These initiatives reflect the NHS’s commitment to leveraging advanced technologies to meet the evolving needs of patients and improve the overall effectiveness of healthcare services.
Funding and Support Initiatives for Digital Health Innovations
To further advance the adoption of digital twins in healthcare, the UK government has introduced a variety of funding initiatives designed to support the development and implementation of digital health technologies. These financial opportunities are intended to encourage innovative solutions that utilise digital twins to enhance patient outcomes and streamline healthcare operations.
One notable programme is the NHS Innovation Accelerator, which provides financial backing to healthcare organisations demonstrating the potential to effectively implement digital twin technologies. By offering grants and resources, the government aims to foster a culture of innovation and collaboration within the healthcare sector, ultimately driving the successful integration of digital twins into routine practices.
Additionally, partnerships with technology firms and academic institutions are being actively encouraged to strengthen research and development efforts focused on digital twins in healthcare. This collaborative approach ensures that diverse expertise is harnessed, paving the way for groundbreaking advancements in patient care and operational efficiency.
Establishing a Regulatory Framework for Digital Twins
As the adoption of digital twins in healthcare expands, establishing a robust regulatory framework is critical to ensuring their safe and ethical utilisation. The UK government has implemented measures to address concerns surrounding data privacy, security, and the ethical implications of employing digital twins in clinical settings.
The General Data Protection Regulation (GDPR) serves as a foundational element of this regulatory framework, ensuring that patient data utilised in digital twin models is managed securely and ethically. By adhering to these regulations, healthcare providers can confidently leverage digital twin technology while safeguarding patient privacy and maintaining compliance.
Moreover, the Medicines and Healthcare products Regulatory Agency (MHRA) is actively developing guidelines for the application of digital health technologies, including digital twins, in clinical practice. This regulatory oversight is essential in promoting safe and responsible innovation in healthcare, ensuring that digital twin applications meet the necessary standards of quality and efficacy.
Encouraging Collaboration Between Industry and Academia
The UK government is committed to fostering collaboration between healthcare providers, technology firms, and academic institutions to drive advancements in digital twin technology. By facilitating partnerships, the government aims to create an ecosystem that supports research, development, and implementation of innovative solutions capable of significantly enhancing healthcare delivery.
For instance, collaborative projects involving universities and NHS trusts are already underway, concentrating on the integration of digital twins into various facets of patient care. These partnerships leverage academic research and industry expertise to formulate practical solutions that address real-world healthcare challenges.
The establishment of innovation hubs, such as the Digital Health and Care Institute in Scotland, exemplifies the UK’s commitment to nurturing a collaborative environment for digital health advancements. These hubs serve as platforms for knowledge sharing, research collaboration, and the development of pilot projects, ultimately accelerating the adoption of transformative technologies like digital twins throughout the healthcare system.
Successful Case Studies of Digital Twins in UK Hospitals
Numerous UK hospitals have commenced the implementation of digital twin technology in innovative manners, showcasing its potential to revolutionise healthcare delivery. These case studies illustrate the effectiveness of innovating with healthcare digital twins in enhancing patient care, optimising operations, and improving health outcomes.
Royal London Hospital’s Groundbreaking Digital Twin Project
At the Royal London Hospital, the adoption of digital twin technology has markedly improved the efficiency of the emergency department. By constructing a digital twin of patient flows, hospital administrators can simulate and analyse how patients navigate the facility, identifying areas of congestion and opportunities for improvement.
The digital twin initiative has enabled staff to visualise patient journeys, leading to more informed decision-making regarding resource allocation and staffing levels. For instance, by understanding peak admission times and the usual duration of patient stays, the hospital has been able to optimise its staffing levels, ensuring that adequate support is available during busy periods.
As a result of these enhancements, the Royal London Hospital has reported substantial reductions in waiting times, leading to an improved overall patient experience. This innovative approach not only streamlines operations but also enhances patient outcomes, demonstrating the tangible benefits of integrating digital twins into healthcare practices.
Manchester University NHS Foundation Trust’s Innovative Use of Digital Twins
The Manchester University NHS Foundation Trust has successfully utilised digital twin technology to enhance surgical planning and improve patient outcomes. By creating digital replicas of patients, surgeons can better simulate potential surgical scenarios, allowing for more precise planning and execution of complex procedures.
This innovative approach has proven particularly advantageous in the realm of orthopaedic surgery, where comprehending a patient’s unique anatomy is critical for achieving successful outcomes. By employing digital twins, surgeons can visualise the surgical site in intricate detail, enabling them to anticipate challenges and tailor their approach accordingly.
Moreover, integrating digital twins into surgical planning has led to improved recovery times for patients. By ensuring that surgeries are meticulously planned and executed with precision, the Manchester University NHS Foundation Trust has observed a reduction in post-operative complications, further illustrating the positive impact of innovating with healthcare digital twins.
Imperial College Healthcare NHS Trust’s Approach to Operational Optimisation
Imperial College Healthcare NHS Trust has proactively sought to optimise hospital operations through the utilisation of digital twins. By modelling patient journeys from admission to discharge, the trust has gained invaluable insights into the factors influencing patient flow and resource utilisation.
This data-driven strategy has allowed the trust to identify inefficiencies and implement changes that enhance the overall patient experience. For example, by analysing patient pathways, the trust has successfully streamlined processes, minimising unnecessary delays and improving communication between various departments.
The successful incorporation of digital twins into operational strategies has resulted in heightened patient satisfaction and improved healthcare delivery. As the NHS continues to embrace digital innovation, the case of Imperial College Healthcare NHS Trust serves as a compelling example of how innovating with healthcare digital twins can lead to significant advancements in patient care and operational efficiency.
Strengthening Collaboration Between UK Universities and Healthcare Providers
Collaboration between universities and healthcare providers in the UK is crucial for advancing the implementation of digital twin technology. Through these partnerships, innovative research and practical applications are driving improvements in patient care and operational efficiency.
The University of Oxford’s Pioneering Digital Twin Research
The University of Oxford is at the forefront of digital twin research, collaborating with healthcare providers to develop models that facilitate personalised medicine. By leveraging advanced data analytics and machine learning techniques, researchers are creating digital twins that accurately represent individual patients’ health profiles.
These digital replicas are being utilised to inform treatment decisions, allowing healthcare professionals to tailor interventions based on a patient’s unique needs. For instance, in the field of oncology, digital twins can simulate how a patient might respond to specific treatments, enabling oncologists to select the most effective therapies.
This collaboration harbours the potential to revolutionise personalised medicine in the UK, transitioning the focus from a one-size-fits-all approach to a more nuanced understanding of patient care. By integrating insights from academic research with practical applications in clinical settings, the University of Oxford is paving the way for innovative advancements in healthcare delivery.
King’s College London’s Innovations in Mental Health Services
King’s College London is actively pursuing digital twin applications aimed at enhancing mental health services. By creating digital models that represent patients’ mental health trajectories, researchers can gain deeper insights into the factors that influence mental well-being.
The digital twin approach allows for the analysis of various treatment modalities and their effectiveness across different patient profiles. This level of granularity empowers mental health professionals to develop tailored interventions that address the specific needs of individuals, ultimately resulting in better treatment outcomes.
Additionally, King’s College London is working in collaboration with local healthcare providers to integrate these innovations into clinical practice. By bridging the gap between academia and healthcare, the institution is ensuring that cutting-edge research translates into meaningful improvements in mental health services across the UK.
Imperial College London’s Innovative Digital Health Projects
Imperial College London is leading advancements in digital twin technology within the healthcare sector through partnerships with NHS trusts. These collaborations focus on developing innovative solutions that leverage digital twins to enhance patient care and operational efficiency.
One notable project involves creating digital twins of healthcare facilities, enabling administrators to simulate patient flows and resource utilisation. This modelling allows hospitals to make data-driven decisions that optimise processes and improve patient experiences.
Moreover, Imperial College London is also exploring the integration of digital twin technology into chronic disease management. By modelling patient health trajectories, researchers can identify potential complications and intervene proactively. This approach has the potential to enhance care for patients with long-term conditions, ultimately improving their quality of life.
Through these collaborations, Imperial College London is demonstrating the power of innovating with healthcare digital twins to drive meaningful advancements in the healthcare landscape, ensuring that the UK remains at the forefront of digital health innovation.
Addressing Challenges and Embracing Opportunities in the Adoption of Digital Twins in the UK
While the advantages of adopting digital twin technology in healthcare are substantial, several challenges must be navigated. Understanding these challenges, along with the corresponding opportunities they present, can inform strategies for successful implementation across the UK.
Prioritising Data Privacy and Security
As digital twins rely heavily on patient data, ensuring the privacy and security of this information is of utmost importance. Concerns regarding data breaches and the ethical implications of utilising sensitive health information must be addressed to cultivate trust in digital twin technology.
The UK’s regulatory framework, including the General Data Protection Regulation (GDPR), provides a solid foundation for protecting patient data. However, healthcare providers must go beyond mere compliance to ensure that data is handled responsibly. This includes investing in robust cybersecurity measures and training staff to understand the risks associated with data breaches.
Furthermore, as digital twin technology evolves, so too will the challenges surrounding data privacy. Healthcare organisations must remain vigilant and adapt their practices to keep pace with advancements in technology, ensuring that patient data is always safeguarded.
Embracing these challenges presents an opportunity for healthcare providers to demonstrate their commitment to data security and patient privacy, ultimately fostering trust and encouraging the adoption of digital twin technology.
Overcoming Integration Challenges with Existing Healthcare Systems
The integration of digital twins with existing healthcare systems presents technical challenges, particularly in legacy environments that may lack the infrastructure to support advanced digital technologies. However, addressing these integration challenges can unlock significant opportunities for innovation.
Healthcare organisations can adopt a phased approach to integration, beginning with pilot projects that focus on specific areas or departments. By demonstrating the value of digital twin technology in these pilot initiatives, organisations can build a compelling case for broader adoption and investment.
Moreover, the integration process allows for a thorough evaluation of existing systems, identifying areas for improvement and optimisation. This iterative approach not only enhances the integration of digital twins but also offers healthcare providers an opportunity to modernise their overall technology infrastructure.
Navigating the challenges of integration presents a pathway for healthcare organisations to enhance operational efficiency and improve patient care through the effective utilisation of digital twin technology.
Developing Training and Skills for Healthcare Professionals
Equipping healthcare professionals with the necessary skills to effectively utilise digital twin technology is vital for successful adoption. The complexity of digital twins necessitates a skilled workforce capable of interpreting data and translating insights into actionable interventions.
To address this challenge, healthcare organisations must prioritise ongoing education and training programmes for their staff. This could involve partnerships with educational institutions and technology providers to develop specialised training modules focused on digital twin applications in clinical settings.
Furthermore, cultivating a culture of innovation within healthcare organisations can inspire staff to embrace new technologies. By creating environments that celebrate continuous learning and experimentation, healthcare providers can empower their workforce to leverage digital twins effectively.
Investing in training and skill development not only enhances the implementation of digital twin technology but also positions healthcare organisations to respond proactively to future advancements in digital health.
Exploring the Future Prospects of Digital Twins in UK Healthcare
The future of digital twins in UK healthcare is promising, with an abundance of opportunities for expansion and innovation. As the technology continues to advance, its integration into various aspects of healthcare delivery is set to transform patient outcomes and operational efficiencies.
Transforming Primary Care Through Digital Twins
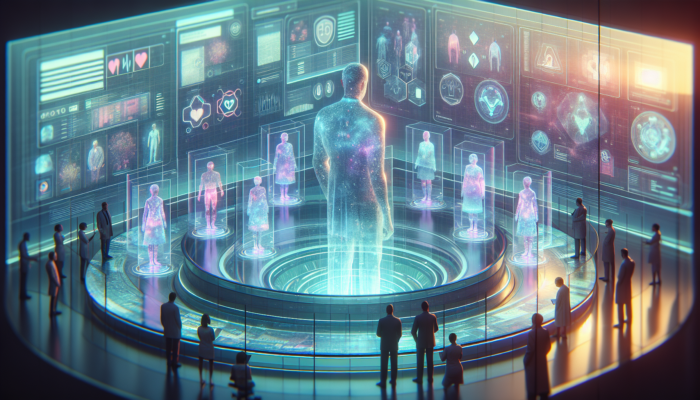
Digital twins have the potential to revolutionise primary care by enabling more effective chronic disease management. By creating digital models of patients with long-term conditions, healthcare providers can monitor health trends and respond proactively to changes in a patient’s condition.
This shift towards a more personalised approach in primary care can lead to significant enhancements in patient outcomes. For instance, by leveraging digital twins, general practitioners can tailor management strategies for patients with diabetes, ensuring that interventions are aligned with individual health profiles.
Moreover, the ability to simulate interventions and predict patient responses can significantly enhance the quality of care in primary settings. As digital twin technology becomes increasingly integrated into primary care, healthcare providers can expect to see reductions in hospital admissions and an overall improvement in population health.
Pioneering Personalised Medicine and Treatment Plans
The widespread utilisation of digital twins in healthcare could herald a new era of personalised medicine and treatment plans throughout the UK. By harnessing individual patient data and digital twin models, clinicians can formulate targeted treatment strategies that take into account the unique characteristics of each patient.
This approach holds substantial implications across various medical fields, including oncology, cardiology, and neurology. By simulating the effects of different therapies on a patient’s digital twin, healthcare professionals can make informed decisions regarding the most suitable treatment options, ultimately enhancing patient outcomes.
As personalised medicine continues to gain traction, the integration of digital twins will be crucial in refining treatment approaches and ensuring that patients receive the best possible care tailored to their specific needs.
Enhancing Public Health Monitoring with Digital Twins
Digital twins could play a pivotal role in monitoring and managing public health crises in the UK. By creating models that simulate population health trends, public health officials can gain valuable insights into disease spread and the effectiveness of various interventions.
For instance, during outbreaks of infectious diseases, digital twins can be utilised to predict how a virus may propagate within communities and evaluate the impact of public health measures. This data-driven approach facilitates more effective resource allocation and targeted interventions, ultimately safeguarding public health.
Furthermore, the integration of digital twins into public health strategies can enhance preparedness for future health crises, ensuring that healthcare systems are better equipped to respond to emerging challenges.
Integrating Digital Twins with Electronic Health Records
Digital twins could significantly augment the functionality of electronic health records (EHRs) in the UK, improving data integration and patient outcomes. By linking digital twins with EHR systems, healthcare providers can create comprehensive profiles that reflect both clinical data and real-time health information.
This integration enables a holistic view of a patient’s health, allowing clinicians to make informed decisions based on the most current data. For instance, by accessing a patient’s digital twin alongside their EHR, healthcare professionals can better comprehend how lifestyle factors impact their health and make adjustments to treatment plans as necessary.
As the healthcare system continues to digitise, the potential for digital twins to enhance EHR functionality represents a significant opportunity for improving patient care and operational efficiency.
Frequently Asked Questions about Digital Twins in Healthcare
What exactly are healthcare digital twins?
Healthcare digital twins are virtual replicas of patients or healthcare systems designed to simulate and analyse health outcomes and operational efficiency.
How do digital twins enhance patient care?
Digital twins improve patient care by enabling personalised treatment plans based on real-time data analysis, resulting in better health outcomes.
What role does the UK government play in the adoption of digital twins?
The UK government facilitates digital twin adoption through funding initiatives, regulatory frameworks, and partnerships with industry and academia to promote innovation in healthcare.
Can digital twins assist with hospital operations?
Yes, digital twins can optimise hospital workflows by identifying bottlenecks and improving resource allocation, which leads to reduced wait times for patients.
What challenges are associated with the adoption of digital twins in healthcare?
Challenges include concerns regarding data privacy, the integration with existing systems, and the necessity for training healthcare staff on new technologies.
How might digital twins transform primary care?
Digital twins can enhance chronic disease management in primary care by enabling more personalised monitoring and intervention strategies tailored to individual patients.
Are there successful case studies of digital twins in UK hospitals?
Yes, hospitals such as the Royal London Hospital and Manchester University NHS Foundation Trust have successfully implemented digital twins to improve patient flow and surgical planning.
What is the future outlook for digital twins in UK healthcare?
The future of digital twins in UK healthcare looks promising, with potential for expansion into primary care, personalised medicine, enhanced public health monitoring, and improved integration with EHRs.
How do digital twins ensure data privacy?
Digital twins comply with regulations such as GDPR, ensuring that patient data is securely managed and ethically utilised to protect privacy.
What skills are necessary for healthcare professionals to effectively work with digital twins?
Healthcare professionals require skills in data analysis, familiarity with technology, and an understanding of how to interpret and apply insights from digital twins in clinical practice.